The Department of Surgery's General Surgery Residency Training Program at the Warren Alpert Medical School of Brown University, is a five-year training program accredited by the Accreditation Council for Graduate Medical Education (ACGME) and approved by the Surgical Residency Review Committee for 35 categorical positions and 10 preliminary positions. There are additional resident trainees who also rotate within our program. Residents from Plastic Surgery, Orthopedic Surgery, Urology, Anesthesia, Neurosurgery, and Emergency Medicine rotate on general surgery rotations and spend anywhere from one month to nine months training in our Program to meet their home program's ACGME specialty required surgical training. The following document will review our curriculum, our methods of assessment, some special features of our program and our outcomes.
Curriculum
The primary goal of the program is to produce superior clinical and academic surgeons who are trained in all facets of modern general surgery.
Breadcrumb
Curriculum
The primary goal of the program is to produce superior clinical and academic surgeons who are trained in all facets of modern general surgery.
Our surgical training program provides a comprehensive education in basic science and core clinical knowledge. It provides cognitive, technical, communication, professionalism, and leadership skills required to excel as a surgeon. All surgical residents receive extensive training in preoperative evaluation in the clinic and hospital settings, intraoperative technique, postoperative, critical care management, and follow up care. Residents rotate through several unique hospitals, allowing for diversity, breadth, and depth of training. In these training settings, the surgical residents are taught, supervised, and evaluated by surgical faculty. Operative and non-operative patient care training is provided with appropriate levels of supervision by faculty members to promote progressive autonomy of trainees that is consistent with Institutional Policies. Supervising faculty promote progressive autonomy of trainees that is consistent with Institutional Policies. Supervising faculty members assess the knowledge and skills of each resident and delegate to the resident's appropriate level of patient care authority and responsibility. Assessment of residents in patient care is guided by specific national standards-based criteria, including milestone designated for general surgery.
In order to prepare residents for the practice of general surgery, or the related surgical subspecialties, we continually re-evaluate and enhance our educational program. The surgical training program has cultivated a robust educational experience for residents not only in basic science and clinical knowledge as applied to the practice of surgery, but also across all the core competencies required by the Accreditation Council for Graduate Medical Education: Patient Care, Medical Knowledge, Practice Based Learning and Improvement, Interpersonal and Communication Skills, Professionalism, and Systems Based Practice.
Our program has followed the web based SCORE curriculum since 2007. Created by The Surgical Council on Resident Education (SCORE), a non-profit consortium formed by the principle organizations involved in U.S. surgical education (American Board of Surgery, American College of Surgeons, American Surgical Association, Association of Program Directors in Surgery, Association for Surgical Education, Residency Review Committee for Surgery, ACGME, Society of American Gastrointestinal and Endoscopic Surgeons). The SCORE curriculum contains patient care topics organized into twenty-eight organ system-based categories which are built-in into a curriculum for a five-year general surgery training program. Topics cover not only the knowledge related to specific disease and operations, but also knowledge of systems and conditions that affect the body as a whole. The Department of Surgery supports individual resident membership for access to the SCORE portal. The SCORE portal is used for supplemental educational content and assessment in support of the curriculum to our trainees. Learning modules are available on the web via the portal, each module features learning objectives, study questions and a variety of resource materials, including textbook chapters, videos, and radiologic images. SCORE learning modules also provide quizzes with multiple choice questions for use in assessing resident knowledge.
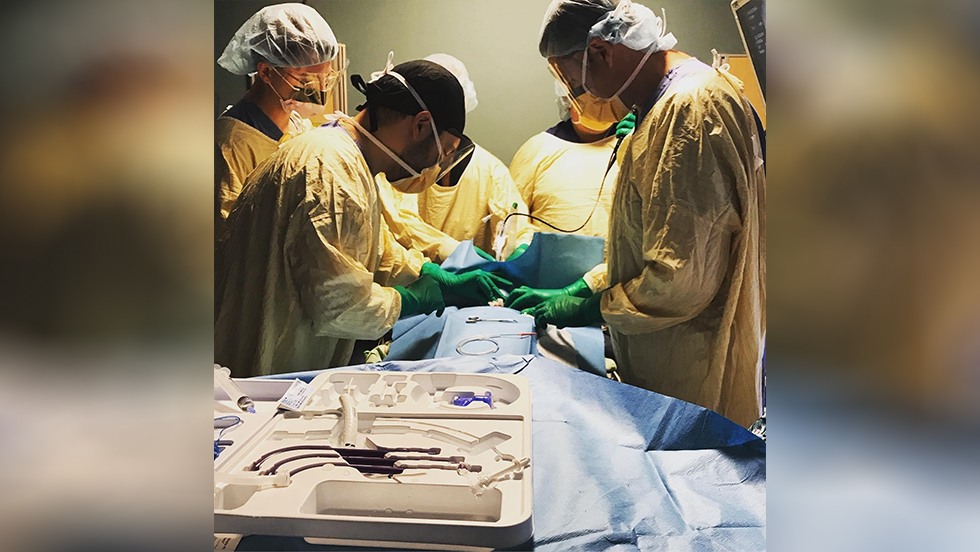
All new PGY 1 residents in our general surgery program participate in the American College of Surgeons Fundamentals of Surgery Curriculum (ACS FSC). The ACS FSC provides incoming PGY 1 residents with basic skills, knowledge, and confidence before they begin their clinical schedule. During the ACS FSC modules, new PGY 1 residents are educated and evaluated on basic patient management such as the evaluation and management of post-operative complications and the evaluation and management of critically ill patients, either immediately post operatively or in the intensive care unit. The PGY 1 residents are also evaluated on procedural competencies such as advanced venous access procedures, tube thoracostomy, and bedside debridement. The ACS FSC also ensures the Program's compliance with the ACGME requirement which states the Program Director must define and demonstrate competencies with a definitive metric for direct and indirect supervision of patient management and procedural competencies.
Our PGY 1 Boot Camp Series is faculty and resident lead, in-depth, one-to-two-hour teaching sessions. These sessions occur twice per week over approximately a ten-week period. Sessions are focused on patient management and procedural competencies. Some examples of session topics are knot tying, surgical nutrition, ventilator management, and central lines.
Incorporation of select simulation training modules, courses, and programs complement our curriculum.
All surgical residents participate in the Advanced Trauma Life Support® (ATLS®) program. Simulating a variety of trauma scenarios, this program teaches residents a systematic, concise approach to the care of a trauma patient. It provides a safe and reliable method for immediate management of injured patients, how to assess a patient’s condition, resuscitate and stabilize him or her, and determine if his or her needs exceed a facility’s capacity. It also addresses how to arrange for a patient’s inter-hospital transfer and assure that optimum care is provided throughout the process.
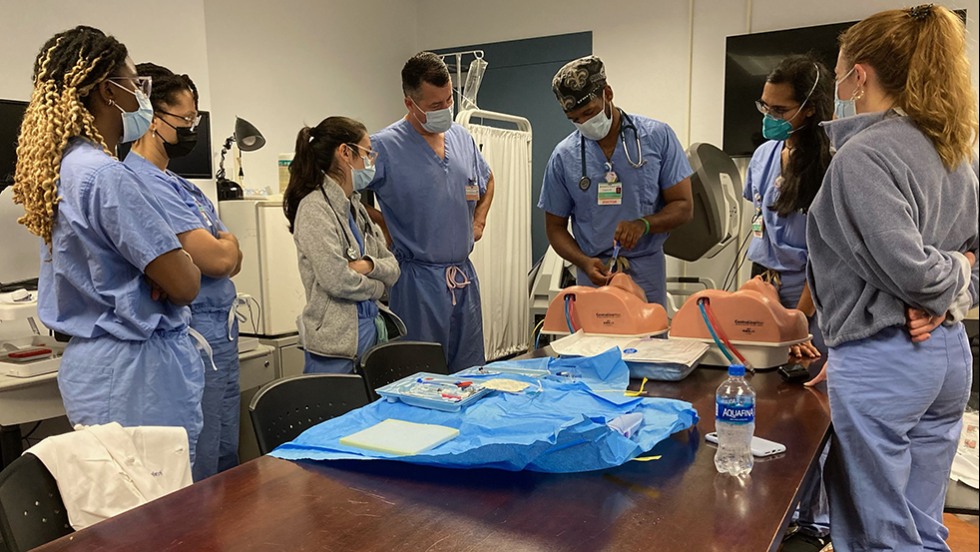
Fundamentals in Laparoscopic Training (FLS) is provided to all residents and a dedicated practice and testing space has been created for resident use. In 2022 the Program purchased three new FLS simulators. The FLS training room is available to all residents 24/7 and is able to accommodate up to three residents practicing simultaneously. PGY 1 residents are provided with an introduction to FLS and FLS level 1 course training. PGY 2, and 3 residents receive FLS level 2 course training and as a PGY 3 the resident is given a pretest on their skills prior to their certification test for Fundamentals of Laparoscopic Training.
Fundamentals of Endoscopic Training (FES) is provided to all residents. The program invested, along with two other departments, in purchasing an Endoscopic Simulator for residents to complete the simulation portions of the FES curriculum. The FES curriculum is spread across the PGY 1, 2, 3, 4 years and as a PGY 4 the resident is given a pretest on their skills prior to their certification test for Fundamentals of Endoscopic Training.
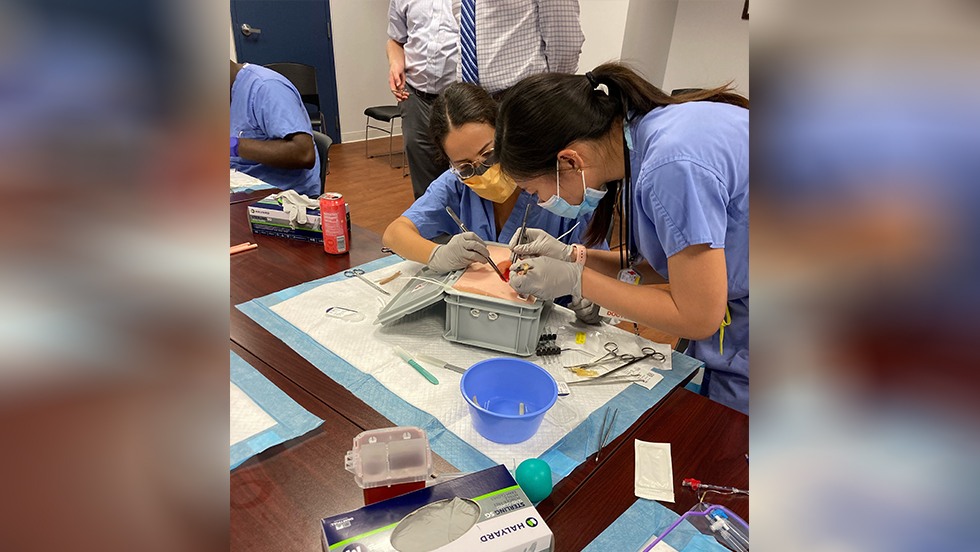
We also have a vascular anastomosis suture lab that was developed here at Brown/RIH. The PGY 2 residents are tested and assessed on this anastomosis model. All sessions are monitored and run by faculty members. Residents are tested providing data regarding the residents’ technical performance and also the progression of an individual resident in technical skills.
Our robotics curriculum is designed to help residents understand the basic components of a robotic operating system, recognize patient safety issues, and become comfortable with basic manipulation of robotic instruments. The curriculum begins during the PGY 1 year. Each resident will complete an Introduction to the Robot session with an educational representative of Intuitive Surgical, complete modules on the simulator, and perform a minimum of 10 bedside assistant cases and 20 console cases with faculty. The Department partners with intuitive to provide a tissue lab at least annually. In June 2022, the Department acquired a simulator for our skills room that can be accessed 24/7 by residents to complete their required modules, additional modules, and operative simulations.
Mock oral examinations are offered to PGY 3, 4, 5 surgical residents through our participation in the New England Mock Oral Exchange Program. This process simulates the American Board of Surgery Oral Certifying Examination. In this program we send faculty members to various training programs as guest examiners and in return receive faculty guest examiners from other Mock Oral Exchange Programs. This factor of the examination - a resident being examined by an attending the resident has never worked with previously - is extremely valuable to provide appropriate levels of realism. Residents are scored in a pass-fail grading system and are provided written feedback and suggestions for improvement on their performance. Metrics generated from this examination are added to the resident's milestones providing the data regarding the resident's level of clinical knowledge and decision-making skills. The resident's aggregated scores are also looked at to identify gaps in our surgery curriculum for the next year.
Junior Mock Oral examinations, similar to the Senior Mock Oral Exams, are offered to PGY 1 & 2 residents. Residents are given simulated case scenarios by PGY 4 & 5 residents and are required to discuss a plan of action and treatment. Residents are scored on a Pass/Fail grading system and are provided written feedback of their performance. PGY 4 & 5 residents are also graded and receive feedback on performance from faculty.
Self-directed learning plays a very important role in physician training. We believe that residents who apply themselves to self-directed learning practices develop educational practices that prove invaluable throughout training as well as during their career as a physician. The Program fosters self-directed learning elements into all assigned curriculum activities and provides multiple resources to allow motivated residents to engage themselves in educational activities. The amount of self-directed learning engagement we expect from residents increases along with the PGY levels.
PGY 1 residents creates a reading schedule for the year, prepares themselves for conferences and rotations by taking advantage of their SCORE membership reading journals and book chapters online, following modules on relevant topics, and taking practice quizzes.
PGY 2 residents begins to develop their research skills, increase their understanding of health care systems, and learn the practice of quality improvement in the development of their outcomes project. They prepare themselves for a more senior role by taking advantage of the assigned SCORE modules. They build upon their reading schedule developed as a PGY 1 resident.
PGY 3 residents independently seek out and work on additional clinical research opportunities above their assigned outcomes project. They utilize all resources available in SCORE to prepare for conferences and rotations. They continue to build their reading schedule and help provide leadership in the running of busy surgical services.
PGY 4 residents take advantage of the skills laboratory to practice their FLS skills independent of assigned practice sessions. They facilitate opportunities to meet with faculty identified as mentors to discuss patient care plans, disease processes, and operations. PGY 4 residents also need to prepare a history of surgery mini-grand rounds to understand the contributions of our surgical forbearers.
PGY 5 residents organize learning opportunities for their team and informal teaching sessions for junior residents. They utilize all resources available in SCORE to prepare for conferences and rotations as well as expanding their reading schedule to prepare for the ABS Qualifying Examination. PGY 5 residents are selected to lead in administrative roles such as Administrative Chief Resident and Quality Improvement Chief. All administrative roles are facilitated and guided by faculty mentors.
In recognition of the need for both clinical and academic physicians in the current and future healthcare environments, the training program offers two tracks of surgical training to our categorical residents. Those residents who wish to purse an academic career may enter into two years of basic science research in one of several research opportunities available within the Department of Surgery. This opportunity occurs after completion of the residents PGY 2 year. Two to three residents per year pursue this track.
For those residents who do not elect a laboratory experience, the clinical track allows for completion of the categorical program in five years with the inclusion of a clinical outcomes research project. It is hoped that this project inspires a lifelong desire of our residents to assess their outcomes in a realistic manner and that this knowledge will make them better physicians. At the end of the first year the resident selects a project they will pursue for two years and a faculty mentor with whom they will collaborate. During the first six months, residents are dedicated to identifying a faculty sponsor, writing a proposal and submitting it to the Institutional IRB. The following twelve months are dedicated to the evaluation of data. The final six months are focused on data analysis and preparation of a presentation to the faculty and fellow residents at a Surgical Grand Rounds at the end of their PGY 3 year. Throughout the resident's experience with an outcome project, they meet multiple times with their faculty mentor for guidance and feedback on their research. All residents submit their outcome projects for presentation at national and regional conferences. Residents are required to attend and provide an update on their project at quarterly meetings. This meeting is much like a bench research laboratory meeting, in that it allows for teaching and mentoring of research topics and allows residents to be peer reviewed of their ideas and formulate solutions to problems encountered. The schedules of outcome project meetings along with the meeting's objectives are set at the start of the academic year. Residents are evaluated midway through this process and a summative final evaluation of their project is completed following their Grand Rounds presentation of their project at the end of PGY 3 year.








PGY 4 general surgery residents are members of the Department of Surgery Quality Improvement Committee and participate in a quality improvement initiative during this year. The general surgery residents are asked evaluate a surgical data base and present their findings at a QI/M&M Conference. Resident preparation for this presentation requires meetings with faculty mentors for guidance and feedback on their assessment of data and presentation of their findings. The Department of Surgery databases available for the 4th year resident to choose from include: NSQIP, UHC, STS, UNOS Trauma 1, BOLD (bariatric).
Surgical residents are encouraged to present their research at national, international and regional meetings.
At Brown, we are deeply committed to your professional development, not only as skilled clinicians but also as exceptional clinician educators. Recognizing the critical role of teaching in graduate medical education, our Residents as Teachers (RaT) program equips the entire resident class with the skills to become effective educators through a comprehensive, longitudinal approach.
Program Structure
Unlike programs that offer sporadic teaching workshops, Brown Surgery integrates educational training into your residency experience. Weekly education conferences include micro-sessions and open group discussions focused on key pedagogical concepts such as feedback, self-assessment, and reflective practice. During procedural simulation workshops, we emphasize strategies like distributive practice, deliberate practice, and models of skill acquisition to build and maintain competency in psychomotor skills. Understanding the rationale behind these methods not only enhances your procedural learning but also strengthens your development as an educator.
Teaching Opportunities
To foster your teaching abilities, we provide a graduated approach tailored to your residency level:
- PGY-1 Residents: You will present to medical students and peers at your level, and participate in select morbidity and mortality discussions, building foundational teaching skills.
- Senior Residents: You will lead presentations for medical students and at educational conferences, as well as deliver talks at department-wide events such as Grand Rounds and Morbidity and Mortality conferences.
Additionally, you will explore innovative curricula delivery methods, such as video-based coaching and podcasting, to diversify your teaching toolkit.
Faculty Mentorship and Feedback
Your presentations will be guided by faculty with specialized training or a strong interest in medical education. These faculty members will:
- Meet with you prior to presentations to review content.
- Provide immediate, documented formative feedback post-presentation to ensure your delivery aligns with adult education principles, enhances participant engagement, and improves understanding of the topic.
Program Goals
By embedding educational concepts from your PGY-1 year and reinforcing them throughout residency, our RaT program aims to graduate residents who are not only proficient clinicians but also confident and skilled clinician educators. This comprehensive training ensures you are well-prepared to teach effectively in academic, clinical, or community settings, embodying the role of a clinician educator.
The resident's clinical experience is complemented by a rigorous academic conference schedule. This schedule is designed to promote resident and faculty advancement in surgical knowledge and is also utilized to develop and hone resident presentation skills in a variety of settings. The interdisciplinary nature of several of the conferences enhances the educational experience and promotes an appreciation for various views and approaches to surgical problems and issues.
Tuesday mornings are designated as academic mornings. During this time residents have three-four hours of protected educational time and are excused from regular patient care activities. In addition to Grand Rounds, all residents are expected to attend Resident Education Conference.
Resident Education Conference is specially designed to teach residents the essential principles and topics of surgery with a focus on high yield ABSITE topics. The beginning of each conference will be ABSITE focused didactics followed by case presentations, questions, operative indication/videos, and/or journal club, etc. Residents are responsible for reviewing current treatment for surgical diseases in preparation for this conference. This conference is overseen by the program directors, Dr. Lynch, and Ashlie Haas-Rodriguez. It is also proctored by faculty members on a rotating basis. Additionally, each PGY 5 will prepare a talk on their assigned topic. Residents will have access to all of the web-based educational resources available through SCORE.
Quality Improvement/Morbidity & Mortality Conference is a department wide, mandatory conference held weekly via In-Person/Zoom. The primary purpose of this forum is to provide quality assurance and peer review. Management complication and outcome improvement are the main emphasis. Discussion is literature based with references provided for each presented case. Presenting residents are expected to create a PowerPoint presentation and are evaluated on the quality of their presentation, understanding of the issues, and on the manner of presentation by the Director of Surgical Education, Program Director, Associate Program Director, or other designated faculty members.
Divisional Service Conferences are held weekly. Residents and students rotating on the service and faculty members of the Division Service participate in these conferences. All Division Service Conferences are directed and proctored by the Division Director, and or designated faculty member. All aspects of patient disease, including pathophysiology, surgical technique, and patient management are addressed and discussed.
The Division of Trauma conference is a weekly conference encompassing the disciplines of Neurosurgery, Orthopedic Surgery, Urology, and Critical Care. The chief resident on the trauma service is responsible for preparation of cases in coordination with the specialty chief resident. Trauma faculty mentors provide guidance and feedback to residents on their presentations. This conference is an interactive format where attending staff review trauma management with all attendees. On the last Tuesday of the month this conference serves as a Quality Improvement/Mortality and Morbidity Conference for the Division of Trauma.
Surgery/ Trauma/ Medicine ICU Combined Conference is a joint conference held weekly. This conference serves as a forum for case presentations of critical care patients and issues. The medical and surgical critical care attendings facilitate discussion amongst the residents regarding intensive care concerns. Residents from the medical, surgical, and trauma intensive care services compare and contrast management plans for critically ill patients.
Trauma and Emergency Medicine Combined Conference is a monthly joint conference with the Trauma Service and Emergency Medicine Department attendings and residents. This conference is an opportunity for both services to explore the management of trauma patients on their arrival to the Emergency Department. Initial assessment, patient management, and communication skills are explored and expanded upon during this conference. Additionally, in-depth review of the evaluation and management of individual trauma patients that have undergone a quality assurance review occurs.
Trauma Morning Report is a daily conference for residents, students rotating on service, the on-call and post-call trauma attending, and Trauma Division attendings. This conference is multifunctional and serves as an educational conference and as a morning sign out. All patients are presented comprehensively by the admitting trauma resident, along with live review of radiologic studies on the PAC system. The History and Physical is updated, completed and signed by the admitting attending following presentation. Additionally, the service listing of patients is reviewed, and the status and care plans are communicated.
Surgical Grand Rounds and special lectureships feature both local, nationally, and internationally recognized faculty. All major areas of surgery are addressed as well as medico-legal and ethical issues. The surgical Grand Rounds audience is comprised of surgical faculty, invited guests, residents, and medical students.
The Department of Surgery hosts five special lectureships within the surgical Grand Rounds series. Each lectureship focuses on a specific area of general surgery. An internationally renowned surgeon is invited and spends two days with our residents and faculty as a Visiting Professor in the Department of Surgery. During this time, the Visiting Professor will address the Department on his/her clinical and research interests, as well as attend a resident round table discussion. Faculty members and research residents present their research and clinical residents present interesting cases to the Visiting Professor. Some lectureships are given annually, and some are semi-annual.
Our program utilizes general surgery milestones to determine resident performance within the six ACGME Core Competencies. General surgery has eighteen milestones which are competency based developmental outcomes that can be demonstrated progressively by residents. Collection of milestone data comes from multiple evaluations and sources. All information is entered into our milestone data base producing an eighteen-point radar plot report on each resident's progress within the six ACGME core competencies. As we are an ACGME accredited training program we are required to appoint a Clinical Competency Committee to review all resident performance data and report their recommendations to the Program Director. The Program has developed a nationally recognized "Radar Plot" organized to summarize the multiple evaluation forms for each resident. Utilization of a radar plot to review the milestone data during the Clinical Competency Committee meetings helps to direct the discussion of each resident's growth. Areas of concern are quickly identified, and Committee members can easily target problem areas to address in their recommendations to program leadership. With the recommendations from the Clinical Competency Committee, the Program Director can then assess the needs of resident learners, implement support, guidance and mentorship where needed and as appropriate for individual residents.
There are many excellent attributes of The Warren Alpert Medical School, Brown University, General Surgery Training Program. A few curriculum elements stand out as unique among our peer training programs.
We are fortunate to have an ACGME and ABS approved international four-week rotation. With our longstanding relationship with Tenwek Hospital, dedicated funding to support resident travel to Tenwek, and commitment of dedicated teaching faculty, we are able to provide a unique, well-structured international elective rotation. Russell E. White, MD, is the Tenwek Medical Mission Hospital's Chief of Surgery. Dr. White graduated from the Brown University General Surgery Training Program in 1995 and holds an academic appointment as a Clinical Professor of Surgery at the Warren Alpert Medical School of Brown University. Dr. White is Board Certified in General Surgery by the American Board of Medical Specialties since 1996. Dr. White is the former program Director of the Tenwek Hospital General Surgical Residency Program which is affiliated with the College of Surgeons of East, Central, and Southern Africa/Pan-African Academy of Christian Surgeons. Dr. White has also been joined by two additional Brown graduates, Robert Parker, MD and Andrea Parker MD. Drs. Robert and Andrea Parker are Clinical Assistant Professors of Surgery at the Warren Alpert Medical School at Brown University. Dr. Andrea Parker is also the Assistant Residency Program Director. This experience is held in Bomet, Kenya at the Tenwek Medical Mission Hospital, and provides trainees with an opportunity to participate in an educational experience that exposes the resident to care for patients with diseases they would rarely see in the United States. Since the Surgery Department at Tenwek is responsible for all subspecialty surgery, the resident obtains operative experience within subspecialty areas of urology, obstetrics, gynecology, plastic surgery, otolaryngology, orthopedic, neurosurgical, thoracic, trauma, and pediatric surgery. The other unique educational characteristic of this elective is the opportunity for resident growth of awareness to the profound societal responsibilities that come with surgical training.
Another unique opportunity that we are able to provide is a 4-week elective rotation at Schneider Regional Medical Center in St. Thomas, US Virgin Islands. This is another great opportunity to provide care to an underserved and rural population. With our relationship with the Schneider Regional Medical Center, dedicated funding to support resident travel to St. Thomas, and committed teaching faculty, we are able to provide a unique and well-structured rural general surgery rotation. Dr. Danielle Comissiong is a general surgery attending at the Schneider Regional Medical Center that works closely with residents and is the site director and primary contact for this rotation. Dr. Comissiong graduated from the Warren Alpert Medical School of Brown University/Rhode Island Hospital General Surgery Training Program in 2022 and holds an academic appointment as a Clinical Instructor in Surgery at the Warren Alpert Medical School of Brown University. Dr. Comissiong is Board Certified in General Surgery by the American Board of Surgery. This experience is held in St. Thomas, US Virgin Islands at the Schneider Regional Medical Center. It provides trainees with an opportunity to participate in an educational experience that exposes the resident to rural surgery and to care for patients with limited resources. In addition to a broad variety of general surgery cases, the experience provides residents with an operative experience within subspecialty areas like urology, obstetrics, gynecology, plastic surgery, otolaryngology, orthopedic, neurosurgical, thoracic, trauma, and pediatric surgery.
We offer selective rotations during the PGY 3 and PGY 4 year. The PGY 3 Selective is designed to allow the resident to participate in a self-selected rotation where they can explore an area of academic interest and broaden their surgical horizon. The PGY 4 Selective is designed to allow the resident to explore a subspecialty in order to gain a better understanding of areas of potential fellowship training they may be considering or gain additional knowledge for the specialty they will be pursuing. Each of these rotation experiences provides the residents with opportunities to identify faculty mentors associated with the resident’s area of interest as well as a dedicated time for self-reflection on their training experience to date and set goals for future training.